Did you ever wonder how ophthalmic diagnostic findings get their names? If you feel like there is no rhyme or reason to the naming conventions used in ophthalmology, you are not alone. Ophthalmology (and medicine in general) does not have structured system of nomenclature like some other sciences.
For example, the field of chemistry utilizes the periodic table of elements to organize and classify fundamental information. Biology employs Linnaean Taxonomy, which is an organized hierarchical system of classification including kingdom, phylum, class, order, family, and genus, to differentiate and name species. It was established and organized by Carl Linnaeus in the mid 1700’s and results in a naming convention known as binomial nomenclature.

In binomial nomenclature, this common Tiger Swallowtail butterfly is known as Papilio Glaucus. It was classified and named by Linnaeus himself in 1758. Papilio is latin for butterfly and glaucus means blue.
Human anatomy and medicine is a different story however. Historically there has been controversy, disagreement, language differences, and confusion amongst anatomists regarding universal terminology. To address this, there have been attempts to standardize terminology in human anatomy. Nomina Anatomica was the international standard on human anatomic terminology from 1956 until it was replaced by Terminologia Anatomica in 1998. But in ophthalmology, as in much of medicine, there is no universal system of classification for ocular anatomy, clinical findings, or diseases. It’s a bit of a “free-for-all”. In the late nineteenth century some 50,000 terms for various body parts were in use. The same structures were described by different names, depending on the anatomist’s background: school, language, culture, traditions, etc.
Let’s take a look at some of the ways that diseases are named in ophthalmology. Clinical findings may be named for their anatomic location, clinical appearance, etiology, disease process, or end result. They may also be based on etymologic roots or finally, eponyms.

A common and logical diagnostic naming convention is simply descriptive of a disease process like vitreomacular traction or corneal erosion.

Or it could be the anatomic result of those processes such as a macular hole that results from vitreomacular traction or a corneal ulcer that arises from erosion.

Some terms are based on clinical appearance, either the literal appearance or a resemblance to something else. Pink eye or floppy lid syndrome are conditions that are literally descriptive of their appearance.

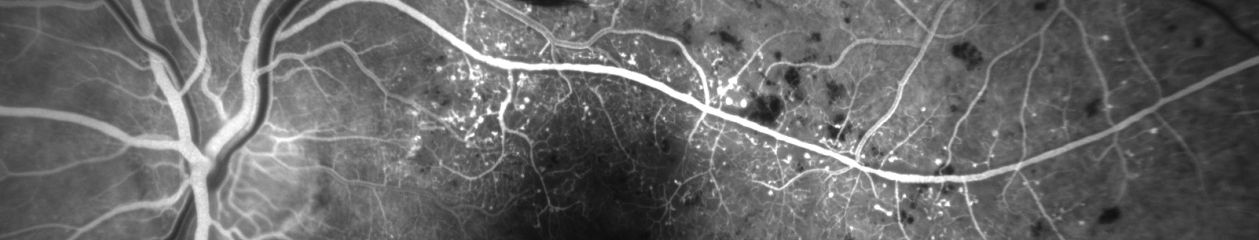
Conditions like bear tracks, bullseye maculopathy, cotton wool spots, morning glory nerve, birdshot choroidopathy, and several others often bear a resemblance to something that would be commonly recognized or understood.

Other names may be based on etymology, which means they originate from traditional Greek or Latin root words. Heterochromia is a good example as it comes from the Greek roots heteros which means different, and chroma which means color.

Cataract is an interesting term that may be related to the opaque lens’ resemblance to rushing water of a waterfall, or possibly to one of the earlier etymologic roots meaning a covering or impediment.
Some conditions are probably better known by the acronym representing the full name: ARN, CHRPE, APMPPE, etc.
Finally, many conditions are based on eponyms meaning they are named for a person, usually the person that first identified or described the condition in the literature. Eponyms are a longstanding tradition in science and medicine, and being awarded an eponym is considered an honor.
Anatomists seem to have been especially fond of naming structures for themselves as seen by the many eponymous anatomic terms in ophthalmology: Bowman’s Membrane, Descemet’s Membrane, Canal of Schlemm, Annulus of Zinn, Schwalbe’s Line, Tenon’s capsule, and Bruch’s Membrane to name just a few.

Eponyms extend beyond anatomy into diagnoses as well. Conditions have been named for Sjögren, Krukenberg, Stargardt, Marfan, Elschnig, Thygeson, Vogt, Cogan and countless others. We certainly shouldn’t overlook Austrian ophthalmologist Ernst Fuchs, who described several conditions and has his eponym associated with many of them. Eponyms may also be proper names of places ( Lyme Disease, North Carolina Macular Dystrophy) or famous patients: Lou Gehrig’s Disease (amyotrophic lateral sclerosis) or Tommy John surgery (named for Major League pitcher, first person to undergo the procedure).
With all these names and egos involved, there has often been confusion and controversy over who was the first to fully describe a condition. Bergmeister’s papilla and Mittendorf dot are eponyms given to remnants of opposite ends of the embryonic hyaloid artery. Vogt-Koyangi-Harada disease is named for three investigators who independently described different manifestations of the same underlying condition. Stevens-Johnson syndrome, named for pediatricians Albert Mason Stevens and Frank Chambliss Johnson, also has several other eponyms associated with it including names such as: Baader, Fiessinger, Rendu, Fuchs, Klauder, Neumann and Hebra – whew! Further confusing things are hyphenated or double surnames such as Robert Foster-Kennedy (Foster-Kennedy syndrome ) and Roger Wyburn-Mason (Wyburn-Mason syndrome).

In fact, Wyburn-Mason syndrome had been previously described in the French literature and is also known as Bonnet-Dechaume-Blanc syndrome. So the correct eponym may depend on what language you speak.
Eponyms are often controversial, especially when questions arise about the moral and ethical character of eponymous honorees. There has been sparring in the literature for years over the use of eponyms and the worthiness of some of the individuals that have conditions named for them. Pulido and Matteson ask the question, “Is it worth having eponyms at all?” in an editorial in Retina in 2010. They go on to state, “Although they can function as a memory aid, they do not enhance understanding of disease…. It is best henceforth to not name new diseases with eponyms and to start moving away from their use completely.”

Wikipedia lists some of the pros and cons of eponyms in eponomously named diseases and briefly talks about current trends:
“The current trend is away from the use of eponymous disease names, towards a medical name that describes either the cause or primary signs.”
“The scientific and medical communities regard it as bad form to attempt to eponymise oneself.”
Then there is Stigler’s Law of Eponymy, which states, “No scientific discovery is named for the original discoverer.” As proof, Stigler freely admits that others postulated the idea before he named it for himself! In describing Stigler’s Law, Malcolm Gladwell stated, “We think we’re pinning medals on heroes. In fact, we’re pinning tails on donkeys.”
David Cogan talked about the pitfalls and limited life of eponymous designations in an editorial in the Archives of Ophthalmology in 1978. Yet Cogan-Reese syndrome was named for him and Algernon Reese many years ago.
 When a new designation, ICE syndrome, was suggested as a unifying term to replace Cogan-Reese syndrome, Chandler syndrome, and essential iris atrophy, Cogan was quoted by William Spencer in another editorial in Archives: “Better a descriptive name, if that is possible, and an eponym if it is not possible. Now the syndrome described by Al Reese and me is characterized by nodules, unilateral glaucoma, Descemet’s membrane and endothelial extension; why not call it by the acronym NUDE syndrome? This would give it sex appeal and put the Archives right up there with Esquire.” Cogan’s response suggests he thought eponyms still have their place – especially when it came to one named for himself!
When a new designation, ICE syndrome, was suggested as a unifying term to replace Cogan-Reese syndrome, Chandler syndrome, and essential iris atrophy, Cogan was quoted by William Spencer in another editorial in Archives: “Better a descriptive name, if that is possible, and an eponym if it is not possible. Now the syndrome described by Al Reese and me is characterized by nodules, unilateral glaucoma, Descemet’s membrane and endothelial extension; why not call it by the acronym NUDE syndrome? This would give it sex appeal and put the Archives right up there with Esquire.” Cogan’s response suggests he thought eponyms still have their place – especially when it came to one named for himself!
Surprisingly, these trends and opinions haven’t prevented the coining of new eponyms in ophthalmology. In 2013, a new anatomic layer of the human cornea was first described by Harminder Dua in the journal Ophthalmology. There was even a big splash in the mainstream scientific news and social media about this exciting new discovery and the investigator who identified it. As you may have already guessed, the finding is called Dua’s layer. He named it for himself!
Despite all the controversies, confusion, and egos involved, it seems as if eponyms in ophthalmology are here to stay, at least for now. So try not to be confused or frustrated when comparing Fuchs’ corneal dystrophy with Fuchs’ heterochromic iridocyclitis, or if you have difficulty remembering whether it is Best’s or Behcet’s disease that has macular vitelliform lesions. We might as well embrace these long-established eponyms – warts and all.
Resources
Here are some great resources to look up information on eponyms in medicine and ophthalmology:
Whonamedit? A dictionary of medical eponyms
http://www.whonamedit.com/
Doyne’s Hall of Fame, Faces behind ophthalmic eponyms
http://www.mrcophth.com/ophthalmologyhalloffame/Doynehalloffame.html
Wikipedia list of eponomously named diseases
https://en.wikipedia.org/wiki/List_of_eponymously_named_diseases
References:
- Whitmore I. Terminologia anatomica: new terminology for the new anatomist. Anat Rec. 1999 Apr 15;257(2):50-3.
- Lamy R, Dantas AM. [Anatomical nomenclature in ophthalmology]. Arq Bras Oftalmol. 2008 May-Jun;71(3):446-58. Portuguese.
- Pulido JS, Matteson EL. Eponyms: what’s in a name? Retina. 2010 Nov-Dec;30(10):1559-60.
- Grzybowski A, Rohrbach JM. “Eponyms: what’s in a name”. Retina. 2011 Jul-Aug;31(7):1439-42; author reply 1442-3.
- Grzybowski A, Rohrbach JM. [Should we abandon the eponym ‘Wegener’s granulomatosis’? A historical excursion]. Klin Monbl Augenheilkd. 2011 Jul;228(7):641-3.
- Dua et al.: Human corneal anatomy redefined: a novel pre-Descemet layer (Dua’s layer) (Ophthalmology 2013;120:1778-85).
- Cogan DG. The rise and fall of eponyms. Arch Ophthalmol. 1978 Dec;96(12):2202-3.
- Eagle RC Jr, Font RL, Yanoff M, Fine BS. Proliferative endotheliopathy with iris abnormalities. The iridocorneal endothelial syndrome. Arch Ophthalmol. 1979 Nov;97(11):2104-11.
- Spencer WH. Proliferating terminology and the NUDE syndrome. Arch Ophthalmol. 1979 Nov;97(11):2103.