Fluorescein angiography records the dynamic interaction of fluorescein with both normal and abnormal anatomic structures of the ocular fundus. A thorough understanding of the circulation phases and appearance of the dye in a normal eye is essential for interpretation of abnormalities. The Normal Angiogram
In a normal eye, the retinal blood vessels and the retinal pigment epithelium both act as barriers to fluorescein leakage within the retina. The tight junctions of the endothelial cells in normal retinal capillaries make them impermeable to fluorescein leakage. The tight cellular junctions of the healthy retinal pigment epithelium provide an outer blood-retinal barrier preventing the normal choroidal leakage from penetrating the retinal tissues.
Additional anatomical features contribute to the interpretation of the fluorescein angiogram. The choriocapillaris is the capillary-rich layer of the choroid characterized by fenestrated capillary walls that leak fluorescein dye freely into the extravascular space within the choroid. In the posterior fundus, the choriocapillaris is arranged in a mosaic of lobules that accounts for the patchy choroidal fluorescence often seen in the early phases of the angiogram. The taller, more pigmented retinal pigment epithelial cells along with the presence of xanthophyll pigment and absence of retinal capillaries in the center of the fovea (foveal avascular zone) contribute to the relative hypofluorescence of the center of the macula.
Phases of an Angiogram
Early Phase
The early phase of the angiogram can be divided into distinct circulation phases that are useful for interpreting the results:

1. Choroidal flush. In a normal patient, the dye appears first in the choroid approximately 10 seconds following injection. The major choroidal vessels are impermeable to fluorescein, but the choriocapillaris leaks fluorescein dye freely into the extravascular space. There is usually little detail in the choroidal flush as the retinal pigment epithelium (RPE) acts as an irregular filter that partially obscures the view of the choroid. If a cilioretinal artery is present, as seen here, it fills along with the choroidal flush as both are supplied by the short posterior ciliary arteries.

2. Arterial phase. The retinal arterioles typically fill one to two seconds after the choroid; therefore, the normal “arm-to-retina” circulation time is approximately 12 seconds. A delay in the arm-to-retina time may reflect a problem with the fluorescein dye injection or circulatory problems with the patient including heart and peripheral vascular disease.

3. Arteriovenous phase. Complete filling of the retinal capillary bed follows the arterial phase and the retinal veins begin to fill. In the early arteriovenous phase, thin columns of fluorescein are visualized along the walls of the larger veins (laminar flow). These columns become wider as the entire lumen fills with dye.

4. Venous phase. Complete filling of the veins occurs over the next ten seconds with maximum vessel fluorescence occurring approximately 30 seconds after injection. The perifoveal capillary network is best visualized in the peak venous phase of the angiogram.
Mid Phase

Also known as the recirculation phase, this occurs about 2 to 4 minutes after injection. The veins and arteries remain roughly equal in brightness. The intensity of fluorescence diminishes slowly during this phase as much of the fluorescein is removed from the bloodstream on the first pass through the kidneys.
Late Phase

The late phase demonstrates the gradual elimination of dye from the retinal and choroidal vasculature. Photographs are typically captured 7 to 15 minutes after injection. Late staining of the optic disc is a normal finding. Any other areas of late hyperfluorescence suggest the presence of an abnormality.
The Abnormal Angiogram
In evaluating diseases of the macula, fluorescein angiography is helpful in detecting abnormalities in blood flow, vascular permeability, the retinal and choroidal vascular patterns, the retinal pigment epithelium, and a variety of other changes.1 Interpretation of the abnormal angiogram relies on the identification of areas that exhibit hypofluorescence or hyperfluorescence. These are descriptive terms that refer to the time-specific, relative brightness of fluorescence in comparison with a normal study.

Hypofluorescence is the reduction or absence of normal fluorescence. Hypofluorescence is caused by either blockage of the normal fluorescence pattern or abnormalities in choroidal or retinal vascular perfusion.

Blocked fluorescence is most commonly caused by blood but can result from the deposition of abnormal materials such as lipid exudate, lipofuscin, xanthophyll pigment or melanin pigment. Fluorescein angiography is very helpful in determining the anatomic location of the blocking material, which in turn, is important in identifying the etiology of the abnormality. For example, preretinal hemorrhage from proliferative diabetic retinopathy blocks visibility of both the retinal and choroidal vasculature while subretinal blood from exudative age-related macular degeneration obscures only the choroidal circulation.

Abnormal vascular perfusion results in hypofluorescence of the retinal and/or choroidal circulation depending on the location of the abnormality. Common causes of retinal hypoperfusion include retinal arterial and venous occlusions and ischemic disease due to diabetes and other causes. Choroidal hypoperfusion may be produced by ophthalmic artery occlusion, giant cell arteritis, and hypertensive choroidopathy. It is important to understand the relationship between hypofluorescence due to filling defects and the specific phase of the angiogram. For example, in many vascular occlusions the hypofluorescence may be a temporary finding until delayed filling of the affected vessel occurs in the later phases of the study.
Hyperfluorescence
Hyperfluorescence is an increase in fluorescence resulting from the increased transmission of normal fluorescence or an abnormal presence of fluorescein at a given time in the angiogram.

Autofluorescence and pseudofluorescence are terms to describe the appearance of apparent hyperfluorescence in the absence of fluorescein. Autofluorescence refers to recordable hyperfluorescence that is believed to occur naturally in certain pathologic entities such as optic nerve drusen and astrocytic hamartomas. Some, but not all disc drusen appear to fluoresce under blue light. Some controversy has existed over whether this is true fluorescence or if there may be a reflective component as well.2 These structures are highly reflective in the same spectral range of fluorescence and could actually be exhibiting pseudofluorescence.


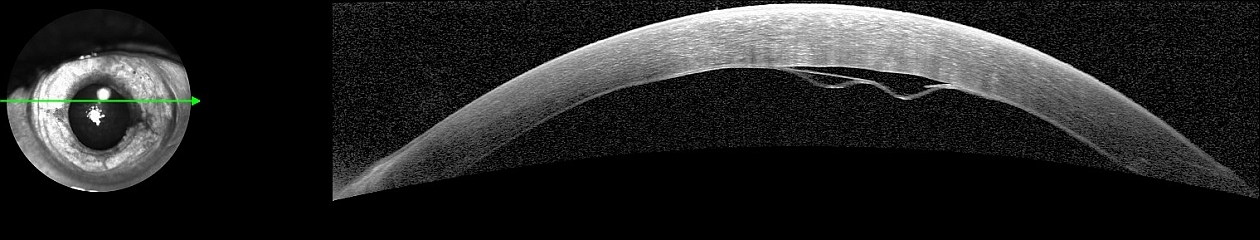
Pseudofluorescence occurs as a result of crossover in the spectral transmission curves of the exciter and barrier filters. If too much crossover is present, reflectance from bright fundus structures will not be fully blocked by the barrier filter and can be seen as noise. Crossover can be the result of mismatched or aging filters. Modern interference filters rarely exhibit significant crossover unless they have deteriorated. Control photographs are routinely taken before injection of fluorescein to detect the possible presence of pseudofluorescence. Left photograph shows slight pseudofluorescence prior to injection (timer at zero). Example on the right demonstrates extreme example with digital gain increased to amplify exposure.
Transmission defect. Depending on the density of retinal pigmentation, background fluorescence from the choroid can be visible as hyperfluorescence in the angiogram. A ‘window defect’ is an area of hyperfluorescence that occurs when there is an absence or reduction of pigmentation due to damage of the retinal pigment epithelium. The loss of pigment allows visualization of the fluorescence created by the underlying choriocapillaris. Window defects remain uniform in size throughout the angiogram. Their brightness rises and falls with the choroidal fluorescence. It is important to differentiate hyperfluorescence due to transmission defects from leakage.


Leakage refers to hyperfluorescence in the angiogram due to extravasation of fluorescein dye. Leakage can result from disruption of the retinal vascular endothelial cell tight junctions or the breakdown of the tight junctions between retinal pigment epithelial cells (the inner and outer blood-retinal barriers, respectively). Examples include macular edema from diabetic retinopathy, cystoid macular edema, and central serous chorioretinopathy. In addition to abnormalities of the retinal vascular system or pigment epithelium, leakage is observed in a variety of conditions associated with the development of new blood vessels. For example, fluorescein leakage is seen in eyes with choroidal neovascularization related to age-related macular degeneration. In these patients, fluorescein angiography is needed to identify the location and features of the choroidal neovascular membrane which, in turn, influences the course of treatment. In eyes with proliferative diabetic retinopathy, optic disc or retinal neovascularization is characterized by intense fluorescein leakage. Leakage can lead to late staining or pooling of dye.

Staining refers to late hyperfluorescence resulting from the accumulation of fluorescein dye into certain tissues. Drusen and chorioretinal scars commonly exhibit staining. Normal staining can occur in the optic nerve and sclera as a result of normal choroidal leakage. Scleral staining is usually only visible when there is a reduction or absence of the pigment epithelium (window defect) and the sclera can be seen clinically.

Pooling is the accumulation of dye within a distinct anatomic space. Pooling can occur in serous detachments of the sensory retina or the retinal pigment epithelium due to a breakdown of the blood-retinal barrier. Central serous chorioretinopathy is a condition that often demonstrates the pooling of fluorescein.
For more on fluorescein angiography, visit:
Fundamentals of Fluorescein
Equipment & Technique
Step-by-Step
References:
- Gass JDM. Stereoscopic Atlas of Macular Diseases: Diagnosis and Treatment, 4th ed. St. Louis, Mosby, 1997.
- Barry C, Singh J, Constable IJ. Are optic disc drusen exhibiting Autofluorescence, pseudofluorescence or reflectance? Journal of Ophthalmic Photography 22:32-35, 2000.